Atopic Dermatitis
Atopic dermatitis is a common skin disease in humans and dogs that is characterized clinically by pruritus (itching). It is a multifactorial disease with immune and skin barrier abnormalities, and a strong influence of genetic, environmental, and nutritional factors.
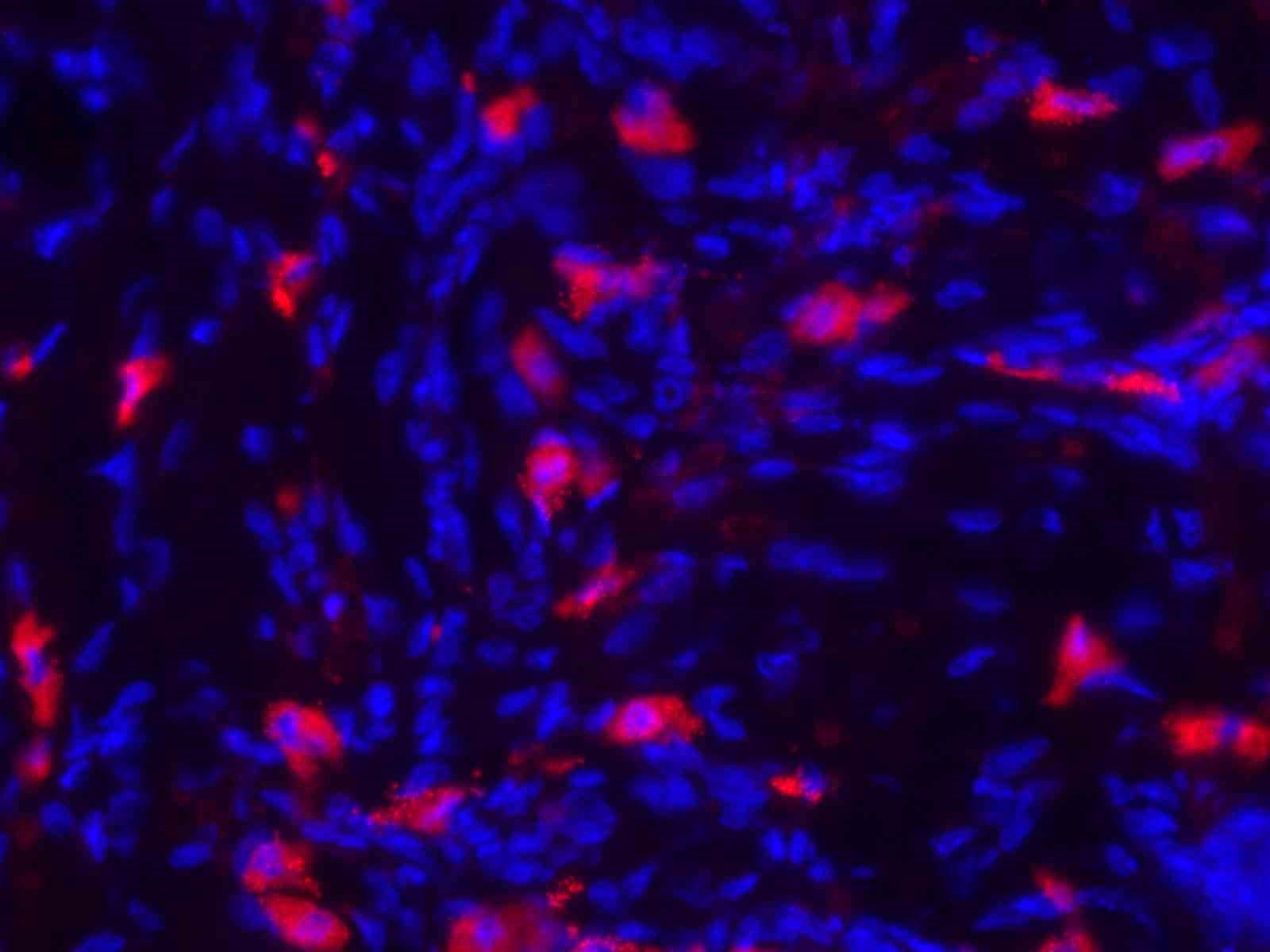
There is accumulation of eosinophils, mast cells, and M2 macrophages in the dermis along with thickening of the epidermis and dermal fibrosis.
Atopic dermatitis is typically driven by Th2 lymphocytes and associated with an increase of IgE antibodies, but recent studies have demonstrated that innate lymphoid cells (ILC2) also contribute and sometimes are the main instigators of type 2 inflammation.
Our initial work focused on a mouse mutant that lacks a protein called SHARPIN. These chronic proliferative dermatitis (cpdm) mice were discovered by us in the early 1990’s. In the absence of SHARPIN, the mice develop a progressive chronic dermatitis with histologic features of atopic dermatitis and an eosinophilic esophagitis at about 4-5 weeks of age. The dermatitis and esophagitis develop in the absence of B and T lymphocytes.
We recently developed a floxed Sharpin mutant and demonstrated that selective deletion of Sharpin in keratinocytes recapitulates the dermatitis.
Atopic dermatitis is associated with changes in the lipid barrier formed by the stratum corneum. Using a shotgun lipidomics approach and multivariate statistical analysis and machine learning, we identified changes in the lipid composition of the epidermis of Sharpin cpdm mice.
We recently conducted similar lipid profiling studies in dogs with the goal to identify sets of lipids (fingerprints) that could serve as biomarkers. This research demonstrated changes in lipids in nonlesional skin and blood which indicates that atopic dermatitis in dogs is associated with systemic changes in lipid metabolism. Treatment with drugs (oclacitinib and lokivetmab) significantly improved the skin condition of the atopic dogs and induced changes in the composition of lipids in skin and blood.
Selected publications
- HogenEsch H, Gijbels MJJ, Offerman E, Van Hooft J, Van Bekkum DW, Zurcher, C (1993) A spontaneous mutation characterized by chronic proliferative dermatitis (cpd) in C57BL/Ka mice. Am J Pathol, 143:972-982.
- Wang Z, Potter CS, Sundberg JP, HogenEsch H (2012) SHARPIN is a key regulator of immune and inflammatory responses. J Cell Mol Med, 16:2271-2279.
- Sundberg JP, Pratt CH, Godwin L, Silva KA, Kennedy VE, Potter CS, Dunham A, Sundberg BA, HogenEsch H (2020) Keratinocyte-specific deletion of SHARPIN induces atopic dermatitis-like inflammation in mice. PLoS One, 15:e0235295.
- Franco J, Rajwa B, Ferreira C, Sundberg JP, HogenEsch H (2020) Influence of sex and disease stage on epidermal lipid profiles in SHARPIN-deficient mice. Metabolites, 10:299.
- Franco J, Rajwa B, Gomes P, HogenEsch H (2021) Local and systemic changes in lipid profile as potential biomarkers for canine atopic dermatitis. Metabolites, 11:670.