Purdue’s Pioneering Procedure Aids a Dog’s Life
Argo the Doberman was in trouble. Diagnosed with ventricular arrhythmia, an abnormal heart rhythm, he was at risk of collapsing and dying at any moment. Although a local specialty clinic had stabilized him, his owner, Dr. Laura Strong (PU DVM ’87), knew that traditional medication wouldn’t be enough.
In her search to give Argo a chance to live a longer life, Dr. Strong returned to her alma mater, the Purdue University College of Veterinary Medicine, which is pioneering a cardiac procedure for dogs.
The Purdue University Veterinary Hospital is one of the few centers in the nation to offer canine cardiac ablation for ventricular arrhythmias, a minimally invasive surgical intervention that treats heart rhythm disorders.
Life threatening arrhythmias in dogs
Dr. Luis Dos Santos, assistant professor of cardiology in the Department of Veterinary Clinical Sciences, is leading the groundbreaking work. His research group, called DARE (Dos Santos Arrhythmia Research Endeavor), conducts advanced research into heart rhythm problems in dogs.
One of the conditions he studies is ventricular arrhythmia, a life-threatening electrical instability that occurs in the heart’s main pumping chambers, causing a dangerously rapid and often ineffective heartbeat. Certain breeds are predisposed to the condition, including Boxers, Doberman Pinschers, and Great Danes.
Dr. Dos Santos aims to uncover the exact reasons why such conditions occur in dogs and then utilize that knowledge to develop more effective, tailored diagnostic tests and therapies. “We need to provide newer options that can treat the heart and provide these animals with a longer survival time, or at least with fewer symptoms,” he says.
Because human hearts are similar to canine ones, his team is seeking possible similarities between humans and dogs, leveraging human heart knowledge and treatments to benefit animal health.
A common procedure in humans
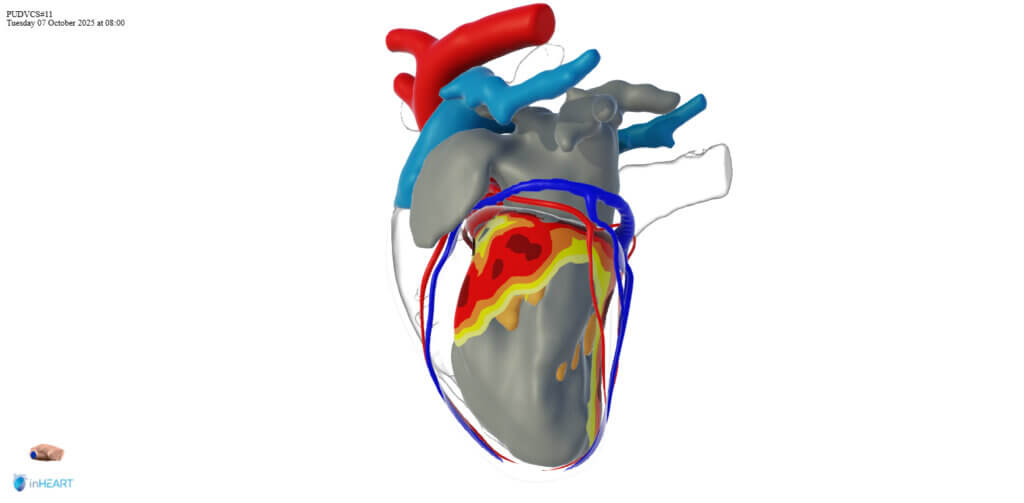
In cardiac ablation, a medical team places catheters inside the heart to precisely map the faulty electrical signals. Then they apply either heat (radiofrequency) or electrical pulses (pulse field) – to a small area of tissue. A tiny scar is created, blocking the errant signals and restoring a normal, healthy heartbeat.
The procedure was first performed on humans in the early 1980s. Since then, it’s become a well-established treatment for abnormal heart rhythms.
As part of his research into canine cardiac arrhythmias, Dr. Dos Santos has been investigating whether cardiac ablation could also help dogs with malignant ventricular arrhythmias.

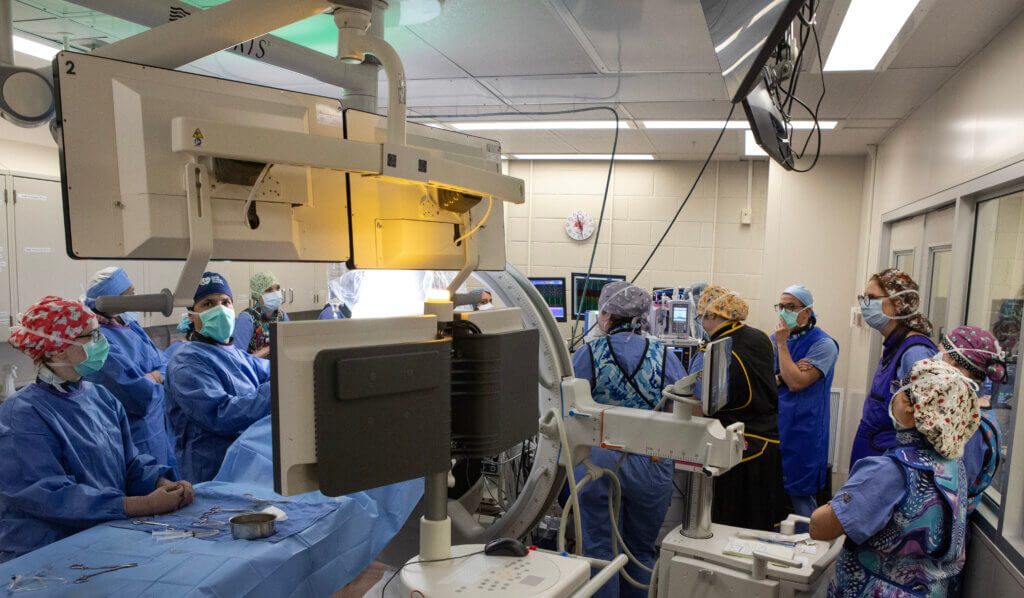
He assembled a team of veterinarians from Purdue and human doctors from Community Health Network in Indianapolis to work on the idea. After perfecting their technique, they waited for the right patients that could benefit from this approach.
Dr. Dos Santos emphasizes the collaborative nature of the work, which unites veterinary and human specialists. “We have an anatomist at the veterinary college, along with radiologists, surgeons, and anesthesiologists. We also have a team of human medical doctors who can come in and help with the procedure. This whole team is supporting and guiding us throughout the process,” he notes.
A key member of the cross-disciplinary team is Dr. Krishna Chaitanya Malineni, a board-certified cardiologist with Community Health Network.
“It is truly remarkable the significant similarities in the anatomy of a dog’s heart to a human being’s heart,” Dr. Malineni says. “The differences are minor enough that once the dog is draped and we are in the heart and mapping and ablating tissue, it almost makes you feel that you are operating in a human heart.”
This collaboration, he observes, benefits both fields. “The cases keep informing me on how to be better for the next case in the human setting as well,” he said.
The cross-disciplinary team’s work is related to Purdue’s One Health initiative, which involves scientific discovery and advancement at the intersection of human, animal and environmental health and well-being.
A veterinarian’s personal quest
For Dr. Strong, former medical director at Eastside Animal Hospital in Jeffersonville, Indiana, the decision to pursue the procedure was rooted in professional knowledge and love for her dog.
“As a veterinarian, I knew Argo was in real trouble when he had his first ‘fainting’ episode at the end of June,” she says. A specialty clinic in Louisville, Kentucky, stabilized Argo initially, and she was grateful for their quick intervention.
“However, with the prospect of sudden death and the probable progression of disease, I wanted to make sure there wasn’t more that we could do,” she adds. “Early interventions improve outcomes, so getting a cardiology consult was a given. I wanted to work with an institution that could provide state-of-the-art cardiac care.”

Through networking, Dr. Strong learned about Dr. Dos Santos’s cardiac ablation procedures. She sent an email to the researcher in July. “Much to my surprise, he responded almost immediately. I was ecstatic,” she recalls. “He kindly answered all my questions, and within two weeks, Argo visited Purdue for a cardiac consult.”
Argo’s owners and the Purdue team discussed the possibility of performing advanced pre-operative cardiac imaging with a gated CT — a specialized scan that takes clear pictures of moving organs.
This produced an unprecedented view of Argo’s heart, showing tissue and structural features in great detail. With this approach, the likely targets of his arrhythmias could be identified before the procedure, which improved preparation for the intervention and increased the chances of a successful outcome.
A nerve-wracking few hours
Despite some medication adjustments, Argo continued to show signs of weakness. “It was clear that medication alone wasn’t going to be enough for long enough,” Dr. Strong says. “Neither my husband nor I were ready for Argo to die suddenly without trying, so when the opportunity for cardiac ablation came along, we were prepared to say yes.”
Leaving Argo the night before was a difficult decision. “My pet owner’s heart wanted a guarantee that Argo would return home with us, and I knew that promise wasn’t possible,” she says. Still, Argo wasn’t afraid to go off with the team, and cardiology specialty intern Dr. Courtney Westcott promised to give the Doberman some kisses.
The morning of the procedure was nerve-wracking. Dr. Strong and her husband, David, grappled with the risks, hoping that Argo would return home with them.
“Ultimately, we had a high level of trust that Argo was in great hands, and we were right,” she says. “Dr. Westcott texted me after a few hours and let us know that Argo had done well. What a relief.”
Back home, Argo had no visible episodes of weakness or collapse, which gave his family some peace of mind.
“One of the challenges of Argo’s heart condition is that a patient can go from seemingly feeling great to sudden death,” Dr. Strong says. “After he had the procedure, Dave and I felt more at ease knowing we were doing everything possible to keep him with us longer.”
As the year drew to a close, the Strongs appreciated the special opportunity they had to be together with Argo through the holidays. Shortly after, they realized those days marked the concluding chapter of his life. Sadly, Argo died suddenly just after the start of the new year.
Light for the Future
With the benefit of this opportunity to utilize the cardiac ablation procedure in treating this condition, Dr. Dos Santos remains committed to providing better options for dogs with arrhythmias, especially given the limitations of currently available drugs.
“Now that we have this group and we are better prepared to manage cases like this, we hope that moving forward we’ll have more cases and become more successful,” he says. Shared mechanisms of the disease between dogs and humans could lead to enhanced techniques that benefit not only canine patients, but also human patients, he adds.

Dr. Strong is grateful that her dog was part of the revolutionary procedure. “Argo’s case hopefully will help to pave the way for other dogs to have life-extending and quality-of-life-extending treatments that target the primary cause of arrhythmias. Perfecting this technique in dogs could be a game-changer for those breeds susceptible to sudden death related to malignant arrhythmias,” she says.
“I’m proud that Purdue is leading the way.”


