Mimicking key features of sporadic Alzheimer’s, the laboratory model shows promise for understanding the disease and testing new treatments.
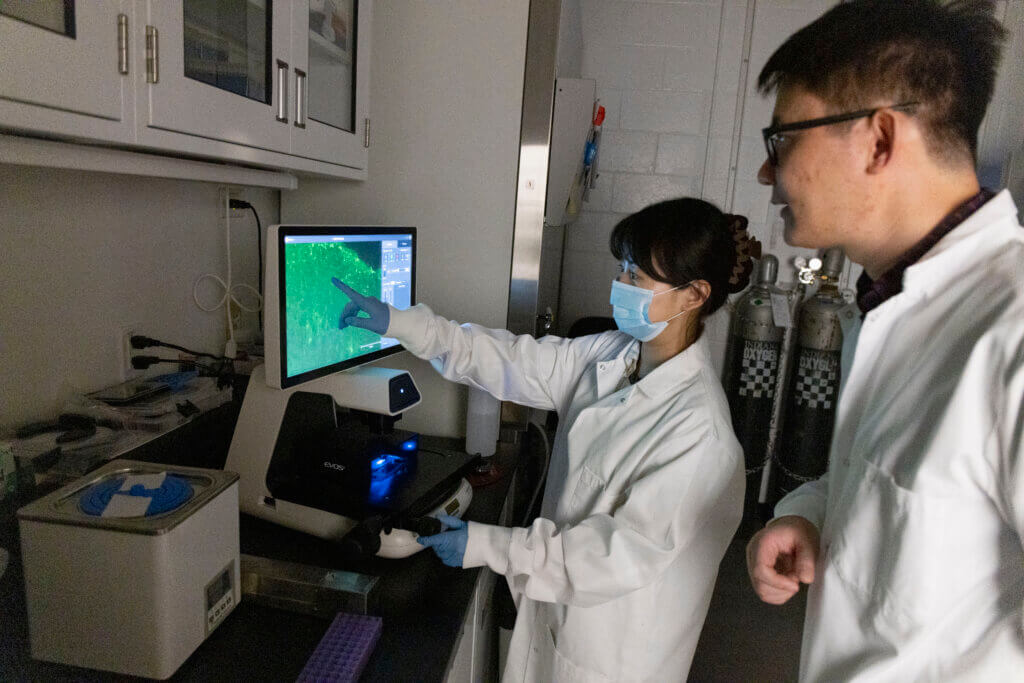
Purdue University College of Veterinary Medicine researchers are taking an innovative approach to studying Alzheimer’s disease. Dr. Ranjie Xu, an assistant professor in the Department of Basic Medical Sciences and a member of the Purdue Institute for Integrative Neuroscience, has developed a sophisticated 3D human mini-brain model to reveal new insights into how the disease progresses and to validate promising new treatments.
This spring, his team published a research article on their findings in the Nature journal Molecular Psychiatry.
A new tool for sporadic AD
The lab’s new tool is an organoid, an artificially grown mass of cells built from human pluripotent stem cells and mimicking the functions of an organ – in this case, the brain. This type of model is often called a “brain on a chip” or “mini-brains” because it’s a miniaturized laboratory system designed to mimic key aspects of the brain’s structure and function.
The researchers developed the tool specifically for studying sporadic Alzheimer’s disease (sAD), which accounts for more than 95% of AD cases and has no clear genetic cause. Most existing research tools are based on familial Alzheimer’s – a much rarer, inherited form of the disease.
While sporadic AD is the prevailing form of Alzheimer’s, it’s influenced by multiple factors, making it difficult to identify causes and patterns.
“Sporadic AD doesn’t have a clear cause. There are no specific gene mutations,” Dr. Xu says. “It’s really hard to get an sAD model. That’s what we wanted to do here in this study.”
A complex 3D model
The model includes four major brain cell types commonly affected in Alzheimer’s – neurons (nerve cells), astrocytes (star-shaped cells that support and protect neurons), microglia (immune cells that protect the brain) and vascular cells (which help maintain the blood-brain barrier, regulate blood flow and coordinate neural activity).
Putting all these brain cells together into a single 3D model can provide a clearer picture of how Alzheimer’s disease affects the brain, says PhD student and lead author Yanru Ji.
“It’s really hard for a single organoid to incorporate multiple different cell types and mimic AD-related pathologies at the same time,” Ji says. “That’s what we did here – incorporate all four different cell types. This helps us better mimic the brain environment.”
Ji is passionate about neuroscience and wants to pursue a career in academia. She read several of Dr. Xu’s publications while looking into graduate programs. Ji says she was drawn to the complexity and unknowns surrounding Alzheimer’s disease, along with the opportunity to participate in his lab’s novel research approaches.
Promising results on multiple fronts
The researchers tested how well the model mimicked the development of Alzheimer’s in humans and how effective it might be in validating new drugs under development. Results on both fronts were promising.
First, the team exposed the laboratory model to brain extracts from postmortem tissues of individuals with sporadic Alzheimer’s. Within just four weeks, the models developed hallmark features of the disease. They included beta amyloid plaque-like buildup (abnormal clumps of protein fragments that disrupt neural function), tau tangles (twisted fibers of tau protein building up inside neurons), brain inflammation, synaptic loss (deterioration and disappearance of connections between neurons) and impaired neural activity.
Given that the model showed these signs of disease so quickly and strongly, the researchers believe it could be a very efficient tool for studying Alzheimer’s.
While longer culturing times might better reflect aging, Ji says that they were able to induce complex pathology in a short timeframe. Their results suggest that the model can efficiently reproduce key features of the aging brain, even in its current form.
A potential model for drug discovery
Next, the team looked at the model’s potential for validating new Alzheimer’s drugs by testing it with lecanemab. Created by Eisai Co., Ltd.; Biogen Inc.; and BioArctic , the drug has been approved by the FDA and is available in the marketplace. It targets beta amyloid, which are believed to damage brain cells and disrupt communication between neurons in people with Alzheimer’s disease.
The medication reduced amyloid levels in the model while also increasing vascular inflammation, closely mirroring human responses.
“This was one of the things we wanted to try with this model,” Ji says. “We want to build a human, physiologically relevant model for testing.”
While the model is still being refined, Dr. Xu says it shows great promise for evaluating new treatments earlier and more effectively. He has applied for a patent via Purdue Research Foundation.
Strong support at Purdue
Dr. Xu received two grants from the National Institutes of Health to support the research project. He also received a Showalter Grant through Purdue’s Office of Research and funding from the Purdue Institute for Integrative Neuroscience. The College of Veterinary Medicine and the Department of Basic Medical Sciences also contributed.
Translational research like Dr. Xu’s aims to bridge the gap between basic science and clinical applications. Dr. Xu says he’s grateful to the university, college, department and the Purdue Institute for Integrative Neuroscience for supporting this kind of bench-to-bedside research, which moves discoveries from the lab to patients faster.
To bolster the team’s ongoing work, the department is outfitting additional space. “Our lab space is relatively limited,” Ji says. A new cell culture room, scheduled to open in the fall, will be located in Lynn Hall near Dr. Xu’s main laboratory. The expansion will allow the team to conduct more experiments and take on bigger projects.
Dr. Xu is currently seeking a postdoctoral researcher to join his team. “We have more exciting work in the future,” he says. The addition of a new researcher signals the growing significance of his team’s work and its potential to provide even more groundbreaking insights into Alzheimer’s disease.

