Aging and obesity may cause stem cells in the body to change in ways that are linked with diseases like Alzheimer’s, diabetes and cancer, according to a study co-authored by scholars at the Purdue University College of Veterinary Medicine and Washington University at St. Louis. The research looked at epigenetic changes — which impact how the body uses its DNA code — in stem cells derived from fat tissue. Results from the study reinforce concerns about the dangers of obesity and raise a warning flag on the therapeutic use of stem cells taken from the fat of people who are obese.
“With obesity, what we’re seeing is that stem cells in fat are primed for disease — they have all sorts of abnormal pathways,” said Dr. Dianne Little, a Purdue University associate professor of basic medical sciences, and joint senior author on the study. “The impact of this priming could apply to the health or otherwise of the heart, the brain, the breast, the gut, because these stem cells live anywhere that there’s fat tissue in the body.”
Dr. Little and her team originally set out to understand whether stem cells derived from fat in obese or older individuals are suitable for use in regenerative medicine. These cells offer attractive advantages as they are generally abundant, and can be differentiated into several different cell types for therapeutic uses. But Dr. Little hypothesized that factors like aging and obesity might cause epigenetic changes that could lead to unanticipated, and potentially detrimental, side effects.
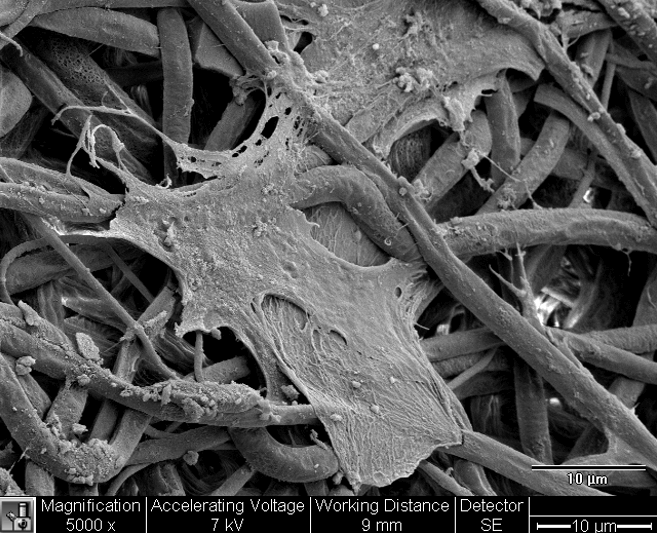
“What we really wanted to know is how do we know if they’re ‘good’ stem cells?” said Dr. Little. “What donor characteristics should we be looking for? If we are an obese or an older adult, would we want our own stem cells derived from fat to be used therapeutically? Are there markers of healthy versus unhealthy stem cells? And if they’re not healthy, what are the detrimental side effects we might get when we use them?”
Inside each of these cells, DNA stores the complete set of instructions used for every component of the body, written in a code made of four nucleic acids attached like the teeth of a zipper on a molecular chain. Two paired strands of DNA are stored zipped together and, throughout the lifetime of the cell, a complex molecular “dance” accesses segments of the strands — genes — that give instructions for assembling specific proteins, or for stopping this assembly process. The term “epigenetic” refers to a group of mechanisms involved in controlling this dance, in which genes are unzipped, copied to messenger RNA, and brought to a cellular factory where the protein is assembled. The epigenome, or how this control system is coded across all of the DNA in the genome, can be influenced by lifestyle and environmental factors during a person’s lifetime, and changes occurring to the epigenome as a result of these factors may be heritable.
Dr. Little investigated the epigenomic mechanism of methylation, a cluster of four atoms that attaches to a link on the DNA chain. DNA methylation sometimes blocks, but can activate transcription of genes at sites where this DNA methylation occurs. In the research published in the journal of the Federation of American Societies for Experimental Biology, her team looked at how obesity and aging impact methylation and then the transcription of associated genes. There is a known link between age and loss of methylation, and indeed, Dr. Little’s team found global loss of methylation on the DNA of stem cells taken from fat in aging, but lean, mice.
However, when they looked at the types of RNA that had been transcribed, or copied, from that DNA, they found only seven genes that were differentially expressed with aging alone. The stability and resilience of the messenger RNA in aging but lean mice indicate that many processes in our cells function properly as we get older despite the loss of methylation, Little said.
Obesity presented a different, and far more troubling story. The messenger RNA of aging and obese mice had more than 800 changes, a 120-fold increase over aging but lean mice. Using existing atlases of genes known to play roles in disease, Little was able to match the messenger RNA sequencing data with known disease pathways.
Dr. Little found that genes impacted by the epigenomic and transcriptomic changes were associated with diseases including Alzheimer’s, diabetes, metabolic disorders, autoimmune diseases, cancer and more.
“The effects of age are dramatically exacerbated when you add obesity into the mix,” Dr. Little said. “These are biological pathways associated with abnormal cell growth, tumors, abnormal cell death. Setting aside the use of these cells in therapies, we have to ask what these cells are doing in their home environment.” Dr. Little said addressing that question will be a focus of her team’s ongoing research.
Entitled, “Aging and Obesity Prime the Methylome and Transcriptome of Adipose Stem Cells for Disease and Dysfunction”, the study was published earlier this year with support from the National Institutes of Health as well as funds from the Duke University School of Medicine and the Purdue University College of Veterinary Medicine. Dr. Little and Dr. Farshid Guilak of Washington University at St. Louis served as joint senior authors, and scientists from Purdue, Duke University, the Frederick National Laboratory for Cancer Research, the University of Rochester, and the University of North Carolina-Chapel Hill also contributed to the research.

