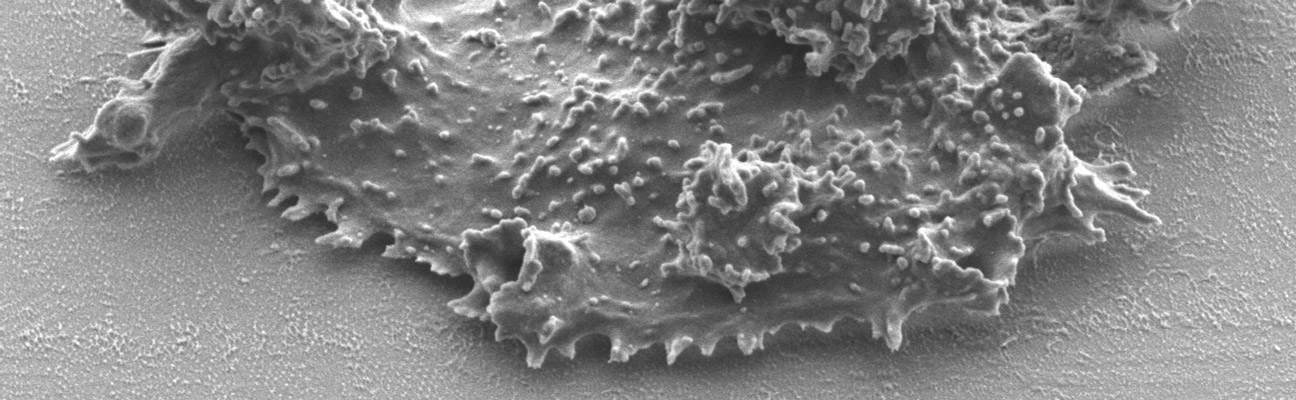
Balamuthia mandrillaris
Balamuthia mandrillaris has a similar pathobiology to Acanthamoeba and is the causative agent of the brain disease Balamuthia amoebic encephalitis (BAE); it has also been reported to cause similar cutaneous amoebiasis. Clinical cases of BAE have been identified with or without cutaneous skin involvement [39]. Since the discovery of B. mandrillaris as an etiological agent in 1986, 108 BAE cases have currently been reported by the CDC between 1974–2016; the clinical cases described in the years prior to 1990 were retrospectively diagnosed [40,41]. Similarly to the other amoebae, the treatment of B. mandrillaris diseases has ultimately revolved around success in a small number of surviving cases and limited in vitro drug susceptibility data. With only 9 successfully treated BAE cases in the US, descriptions of successful combinational chemotherapies include antifungal azoles (ketoconazole, fluconazole, or voriconazole), antifungals (amphotericin B, flucytosine or pentamidine isethionate), antibiotics (azithromycin, ceftriaxone, clarithromycin, ethambutol, isoniazid, rifampin, trimethoprim/sulfamethoxazole, sulfadiazine, pyrazinamide, doxycycline, metronidazole, or minocycline), antiparasitics (albendazole or miltefosine), steroids (prednisolone, dexamethasone, clobetasol propionate), antipsychotics (trifluoperazine, thioridizine) and antivirals (acyclovir). The most recent survivor in 2014 was treated in combination with albendazole, liposomal amphotericin B, azithromycin, clarithromycin, fluconazole, flucytosine, sulfadiazine and miltefosine, highlighting the fact that some of the drugs described in the aforementioned combinational cocktail were used for suspected and misdiagnosed bacterial or viral meningitis. To further complicate treatments, both the infective and destructive trophozoite stage and the dormant cyst stage of B. mandrillaris have been identified during infections.
These high mortality rates indicate that there is a significant unmet medical need to discover new drugs that are efficacious against Naegleria, Acanthamoeba and Balamuthia trophozoites and/or cysts and have increased selectivity to the pathogen over infected dead-end host. Given the lack of major pharmaceutical company involvement in discovery of new drugs for the diseases caused by amoebae, our drug repurposing and development approaches are vital to overcome the unmet medical needs.