Greater understanding of protein aggregation relative to aging is one small step toward slowing or even reversing neurogenerative diseases
Despite more than six decades of research in the field of neuroscience, many functions of the brain — the most complex organ in the human body — remain a mystery. Recent research conducted in the Purdue University College of Veterinary Medicine and the Bindley Bioscience Center revealed that scientists are one step closer to understanding the process that activates and deactivates specific proteins within our cells. This breakthrough could one day lead to enhanced treatments that may slow down or perhaps reverse the advance of neurogenerative diseases such as Alzheimer’s, Parkinson’s and multiple sclerosis.
The key lies in understanding what causes specific proteins to alter their function as we age. Previous studies have established a link between the phosphorylation of certain proteins to different neurological disorders. Phosphorylation is a biochemical process that adds a phosphate to a protein molecule, which often changes the structure and function of the protein. Phosphorylation is the most important mechanism for regulating and controlling protein function and activity as well as transmitting signals throughout the cell.
Through phosphorylation, many brain proteins begin to aggregate by abnormally clumping together. Protein aggregation causes death or injury to cells and is a common characteristic of many neurodegenerative diseases. What is unknown is why phosphorylation causes aggregation in some proteins and not others, and why aggregation tends to worsen as we age.
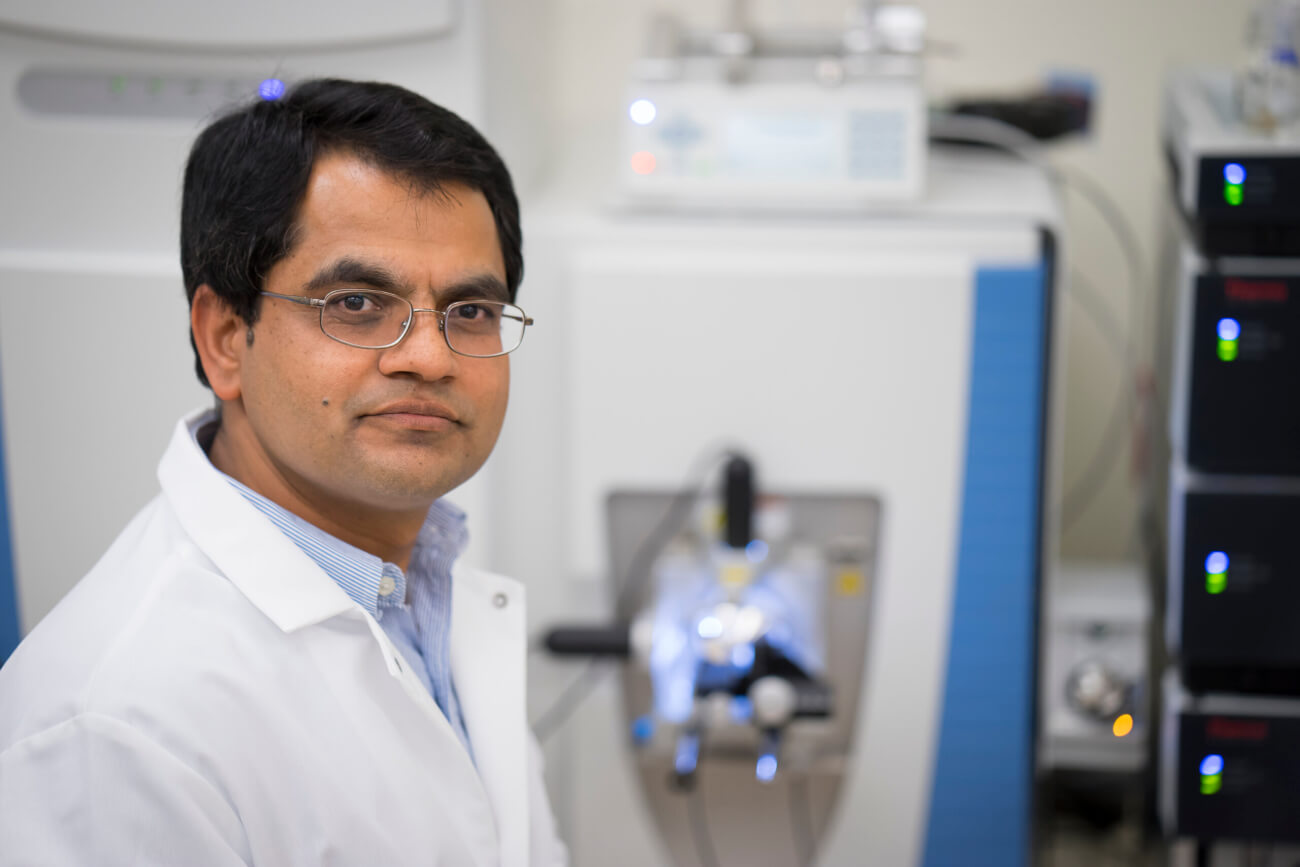
“We wanted to take a deep look into the function of proteins because they are the workhorse of the cell,” says Uma K. Aryal, research associate professor in the Department of Comparative Pathobiology and director of the Purdue Proteomics Facility in the Bindley Bioscience Center. “Understanding the underlying mechanism of these proteins will help us to identify molecular signatures linked to Alzheimer’s, Parkinson’s and other neurological disorders.”
In a study published in the September 2024 journal Molecular & Cellular Proteomics, Aryal, Allison Schaser, an assistant professor of speech language and hearing sciences in Purdue’s College of Health and Human Sciences, and Rodrigo Mohallem (BS ’20), a graduate research assistant and PhD candidate in Aryal’s lab, identified several new molecular markers for neurodegenerative diseases, giving scientists a better understanding about the disease development mechanism and the various pathways by which they develop.
Aryal served as principal investigator for the study and Mohallem ran the experiments. To assess changes in proteins respective to age, they conducted experiments by analyzing animal tissue.
Funding for the project was provided partially by the Indiana Clinical and Translational Science Institute and the Showalter Trust Fund as well as a graduate assistantship from the Bindley Bioscience Center. The research was facilitated by the $3.5 million investment in proteomics equipment by the Office of Research to furnish the Purdue Proteomics Facility. The mass spectrometry instruments are available to researchers across campus.
Using the proteomic and phosphoproteomic technologies available in the Bindley Bioscience Center, Mohallem analyzed thousands of proteins simultaneously. Aryal likens the structure of a protein to a string of different colored beads, where each bead represents an amino acid residue. The arrangement of the beads affects the function of the necklace, just like the specific sequence of amino acids in a protein determine its shape and function. Start moving beads around, and the protein’s properties and function can be altered significantly. In proteomics — the study of proteins — the string is cut, the beads are sliced up and analyzed individually using mass spectrometry, then the necklace is reassembled.
“It’s a kind of reverse engineering,” Aryal says. “Through this process, we collect a lot of information about how the characteristics and functions of the protein might change when its structure is altered. We then use this information to map the effects of phosphorylation within certain proteins.”
Although the tau protein has been very well-studied and was first linked to Alzheimer’s disease in the mid-1980s, the Purdue researchers identified two novel phosphorylated sites on the tau protein that had not been reported before. They also discovered that the two sites within the same protein behaved differently. On one site, phosphorylation decreased with age, while the other site increased. It’s almost like an internal battle within the cell, where one part of the protein is driving toward developing a disease like Alzheimer’s, and another part of the protein is attempting to protect against it.
“There are so many ways phosphorylation can occur within a protein,” Aryal says. “I call proteins a community molecule because they do not function in isolation. If you were to remove a person from their community and drop them off far away in a completely new environment, it would take them time to adapt and learn how to function. Proteins are the same. The same protein cannot function in every part of the cell. Changing their environment alters, or in some cases, inhibits their function.”
The researchers’ discoveries have the potential to propel new scientific developments for the betterment of human health and longevity.
“Our phosphoproteomic study uncovered numerous previously unidentified phosphoproteins and phosphorylation sites, shedding light on age-related changes in brain proteins and pathways that increase vulnerability to neurodegenerative diseases,” says Schaser. “This research is significant, as it may lead to new therapeutic targets for conditions like Parkinson’s and Alzheimer’s.”
The researchers also mapped several kinases, the enzymes involved in phosphorylation that speed up chemical reactions in the body. When a phosphate binds to the protein in an amino acid residue, it’s not a random event. There is a biological process occurring. By identifying the kinases involved in phosphorylation, scientists can begin to determine the mechanism that causes phosphates to bind to certain regions of the protein sequence and not others.
“In the context of neurodegenerative diseases, there is growing interest in kinase inhibitors as potential therapies because kinases play an important role in protein phosphorylation,” Aryal says. “Some kinase-based drugs activate kinases to reduce the severity of the disease. Others inhibit kinases activity to prevent phosphorylation from occurring. By identifying the kinases involved in phosphorylating specific proteins, we can use this information to develop targeted and effective drugs to stop phosphorylation and aggregation. That means there is the possibility that someday in the not-too-distant future, we will have medications available to slow down and even reverse neurodegenerative diseases.”
The initial symptoms of neurodegenerative diseases often manifest differently across people. Some people with Parkinson’s might experience dementia that increases in severity as the disease progresses, while others show no signs of memory loss. Another person could start losing motor control, affecting their ability to walk, while yet another could experience problems with speaking. Each of these symptoms is tied to a different region of brain function, even though all are indicators of the same disease.
Aryal, in collaboration with Schaser, wants to build on this research by identifying in which region of the brain protein aggregation first happens and how it spreads to other regions. He also wants to determine why some cells are negatively impacted by aggregation when others are not. Obtaining cell type specific information, as well as brain region specific information, about these proteins, their phosphorylation and their aggregation, will be critical to understanding the disease mechanisms, and eventually, treating them.
“There are still many things we don’t know about these diseases,” Aryal says. “That’s what’s exciting. This discovery will prompt scientists to start thinking differently than they used to think before.”